Today is World Obesity Day. Obesity is on the rise globally. According to World Obesity Day, 1.9 billion people around the world will be living with obesity by 2035. Efforts to address obesity are challenging due to misconceptions about obesity and the role it plays in a person’s health. For some, exercise plays a big role in weight loss. However, access to exercise facilities and services is not readily available. A recent Survey on arthritis and exercise conducted by Arthritis Consumer Experts (ACE) identified barriers people living with arthritis may face when seeking exercise guidance and support from health care providers.
In 2018, the European Alliance of Associations for Rheumatology (EULAR) updated its recommendations for physical activity in people living with inflammatory arthritis and osteoarthritis. Physical activity is defined as any movement that is produced by the muscles that requires energy (i.e., any movement a person does). Physical activity includes exercise, sports, and physical activities done during daily living, such as gardening and active transportation. Exercise is planned, structured and repetitive activity with the goal to improve or maintain one’s physical fitness.
The EULAR guidelines for people aged 18-65 years living with arthritis are:
- Do moderate intensity aerobic physical activity for 30 minutes or 5 days per week; or,
- Do vigorous intensity aerobic activity for 20 minutes or 3 days per week.
These guidelines can be adapted for someone living with rheumatoid arthritis, osteoarthritis, and spondyloarthritis.
It is important that health care providers help their clients work exercise into their daily routine, understanding that they already spend time self-caring for their disease. Adding or increasing time spent for exercise can prove challenging for some.1
While the research literature tells us a lot about exercise, it is important to hear directly from people with arthritis. ACE conducted a Survey, from March 16, 2022 to April 5, 2022, to learn more about peoples’ exercise routines and preferences before and after their arthritis diagnosis and identify any barriers they have experienced when seeking exercise guidance and support from health care providers.
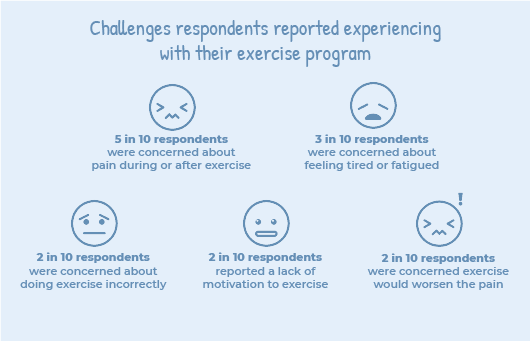
Below are some challenges reported by Survey respondents:
What you can do
In terms of exercise, remember that some is better than none. Over time, taking the stairs or going for a brisk walk around the block adds up. If you are engaged in sports or activities that you do not want to give up, bring it up and speak honestly with your HCPs about your desires and needs. Keep in mind that you may have to compromise or modify how you do certain activities, but you do not necessarily have to give them up. If you are completely new to exercise or getting back into it, then start small and work on consistency before you move on. For instance, do ten push ups at your counter while waiting for your kettle to boil and do it every day until it becomes a habit. Lastly, ask yourself what knowledge and skills do I need to learn? Where do I go to gain access to programs and resources? And who can support me on my journey? Use this information to build a sustainable exercise plan. As with weather, plan for the worst but hope for the best.
Read the full Survey report here.
Resources for your exercise journey
To help you on your exercise journey, the following resources may be helpful: